By Erica Gambarotto, Registered Physiotherapy
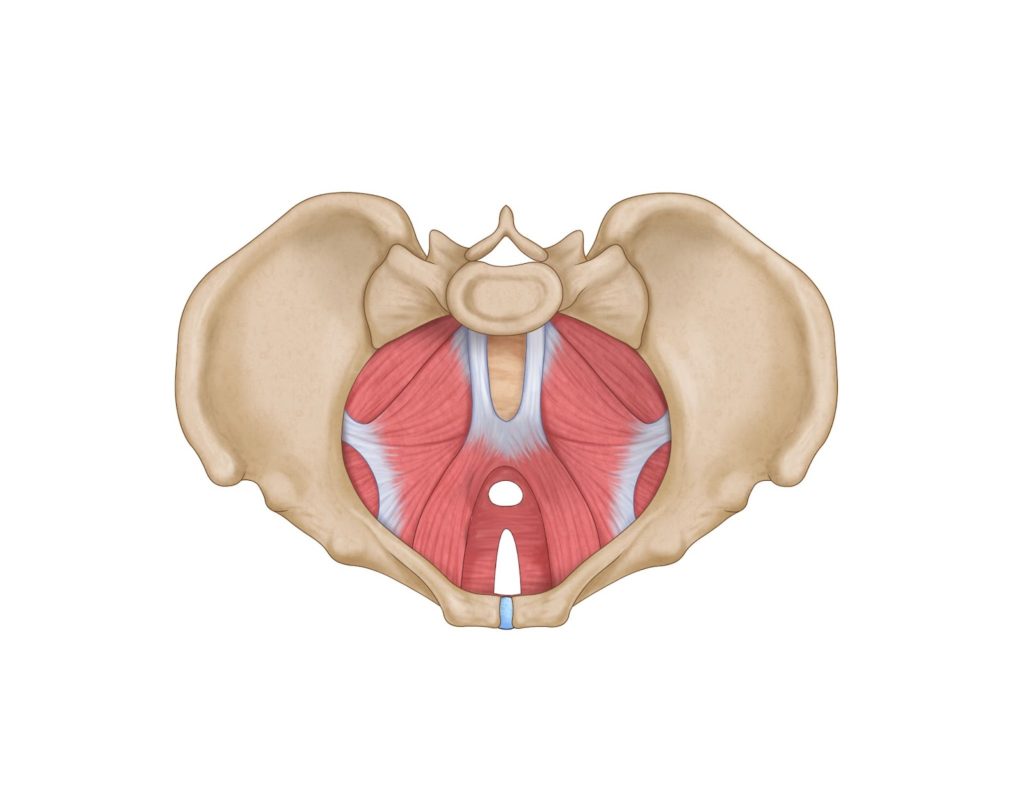
The pelvic floor consists of a group of muscles and connective tissue comprised of 3 layers, the deepest
of which lines the inside of your pelvis and cannot be touched from the outside. These muscles work
together as a sling that span from the tailbone to the pubic bone and from each ischial tuberosity (the
bones that you sit on just under your buttocks).
Pelvic floor muscles perform 5 important functions: they hold up your organs; keep pee and poo off the
floor; assist with stabilizing your pelvis and trunk with your core; allow you to orgasm; and act as a sump
pump to help return blood and lymph back up towards the heart.
Kegels describe a voluntary pelvic floor contraction. The term “Kegels” was first coined by Arnold Kegel,
an American gynecologist, who began using pelvic floor exercises as a conservative means to treat
incontinence. Today, pelvic floor exercises are an evidence based, effective means to treat incontinence,
pelvic organ prolapse and a variety of other forms of pelvic floor dysfunction.
Clients frequently ask me about a video they saw on YouTube or a handout they received from a
doctor’s office detailing how to do various post-partum exercises. Typically this involves the client
performing Kegels by practicing “stopping pee” or “stopping gas” contractions on or off the toilet. There
are several problems with this for several reasons.
The Society of Obstetricians/Gynecologists of Canada recommend that pelvic floor training should be
done only with digital palpation or biofeedback. In other words, pelvic floor retraining should not be
given without internal palpation of the pelvic floor muscles.
There are a few reasons for this:
- Even with verbal or written direction, people perform Kegels inappropriately. For example,
someone may overuse their abdominal muscles or hip muscles instead of their pelvic floor. You
may not know that you are performing the wrong contractions because the pelvic floor cannot
be seen. Therefore, the wrong contraction is repeated indefinitely and may create problems
elsewhere. - The vast majority of the pelvic floors we assess as pelvic health physiotherapists are in fact
OVERACTIVE. An overactive pelvic floor can be associated with urinary urgency, stress
incontinence, pelvic pain, tailbone pain, low back pain, hip pain, and painful sex. Individuals with
an overactive floor who practice Kegels risk worsening their symptoms. By being assessed
internally by a pelvic physiotherapist, they can determine whether or not your pelvic floor
requires strengthening or relaxation. Remember that a large percentage of the people we assess
actually have great fundamental strength but lack control and the ability to relax fully. - The recommendation to practice “stopping pee” on the toilet is a risky practice as it can increase
your chances of experiencing a urinary tract infection. This may be done infrequently to test
control.
In summary, the pelvic floor is an incredibly complex but often overlooked system that is integral to our
health and wellbeing. Written or verbal instructions are often insufficient for those who suffer from
pelvic floor dysfunction. If you have tried Kegels at home with no help or worsening symptoms, this is a
great indication that further investigation is warranted.
As to which exercises are good for versus dangerous for the pelvic floor, again, there is no black and
white answer to this question. It often depends on the client’s individual circumstances (for example,
history of vaginal childbirth, obesity, activity level, pelvic floor strength, etc). Generally, when trying out
a new exercise or exercise program, you can monitor your symptoms to determine if it is a right fit for
you.
If you experience an increase in or onset of the following, this is a sure sign that your body does not
like the new exercise:
low back pain, hip pain, abdominal pain, vaginal or rectal pain
incontinence (either leaking with coughing, laughing, or sneezing OR leaking associated with
urgency)
pain with intercourse
vaginal heaviness
In general, a good way to protect the pelvic floor during exercise is to breathe and contract the pelvic
floor when exerting yourself. Never hold your breath as this creates a strong downwards pressure within
your abdomen and pelvis which can increase your risk of pelvic organ prolapse and incontinence. If you
are unsure of how to contract your pelvic floor or have tried repeatedly with worsening symptoms,
contact your local pelvic physiotherapist who can guide you through this isolation and develop an
exercise program tailored to you and your needs.